Chronic Pain Syndrome:
Symptoms, Causes, Diagnosis and Treatment
That ski trip tumble, the Christmas Day mishap, Sports injury or an unfortunate fender bender, stomach bug or something more serious. All scary, painful but luckily not immediately life threatening. After a few days of recovery, you try to go back to your normal life but the pain is still there, still lingering. Unfortunately, it may come after a cancer or arthritis diagnosis or you can’t even pinpoint the exact time because it was a slow gradual stiffening and you’ve always been delicate.
After a month of ignoring it you decide to take some over the counter pain meds and tolerate it some more. By the time you realize that this is not working anymore it’s been three months already. From the time you book an appointment to the time you see your healthcare professional and have an actual diagnosis you’re in pain for six (6) months, maybe more.
Not only are you now in pain there are other psychological, mental, physical and financial constraints as well. You are desperate as you crawl your way over to the office and slump down in that chair thinking: “Please, make it go away!”
The pain, sadness and guilt that you feel for having the life you knew taken away from you compounds and you begin to feel more anxious and depressed and this causes you to decline invitations, stay in more. Your sleep pattern is now off because you’re in PAIN! So now you’re tired all the time, maybe an insomniac, even?
Phone on silent, curtains drawn, PJs are now the outfit of the day.
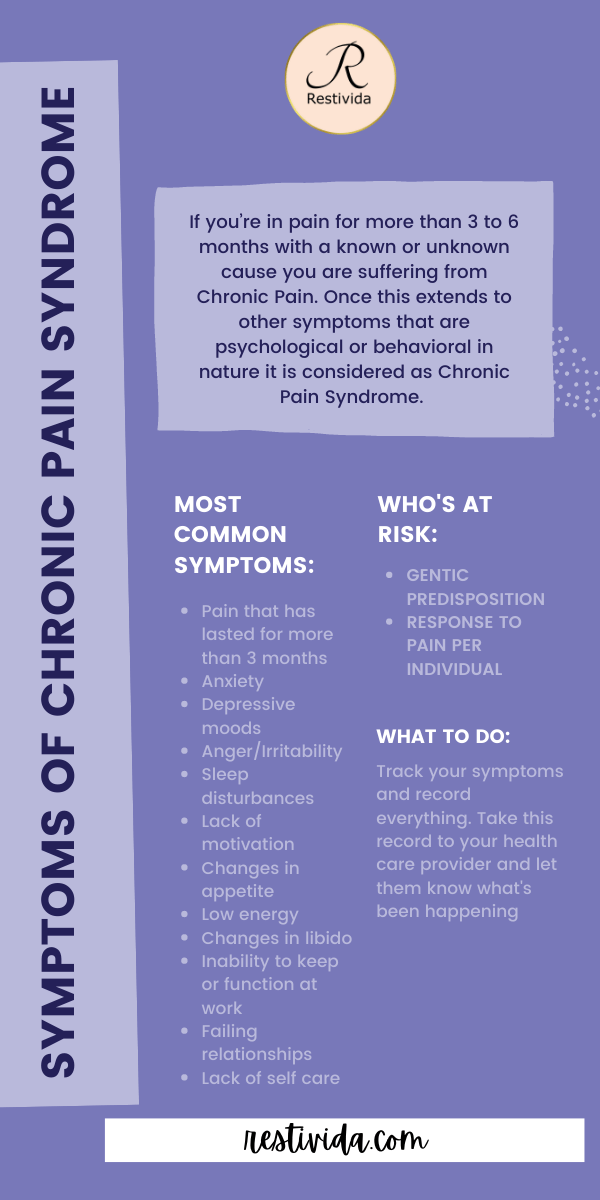
If you’re in pain for more than 3 to 6 months with a known or unknown cause you are suffering from Chronic Pain. Once this extends to other symptoms that are psychological or behavioral in nature it is considered as Chronic Pain Syndrome.
The word “Syndrome” meaning a number of symptoms all happening at once that is used to diagnose or classify certain diseases.
Symptoms of Chronic Pain Syndrome
- Pain that has lasted for more than 3 months
- Anxiety
- Depressive moods
- Anger/Irritability
- Sleep disturbances
- Lack of motivation
- Changes in appetite
- Low energy
- Changes in libido
- Inability to keep or function at work
- Failing relationships
- Lack of self care
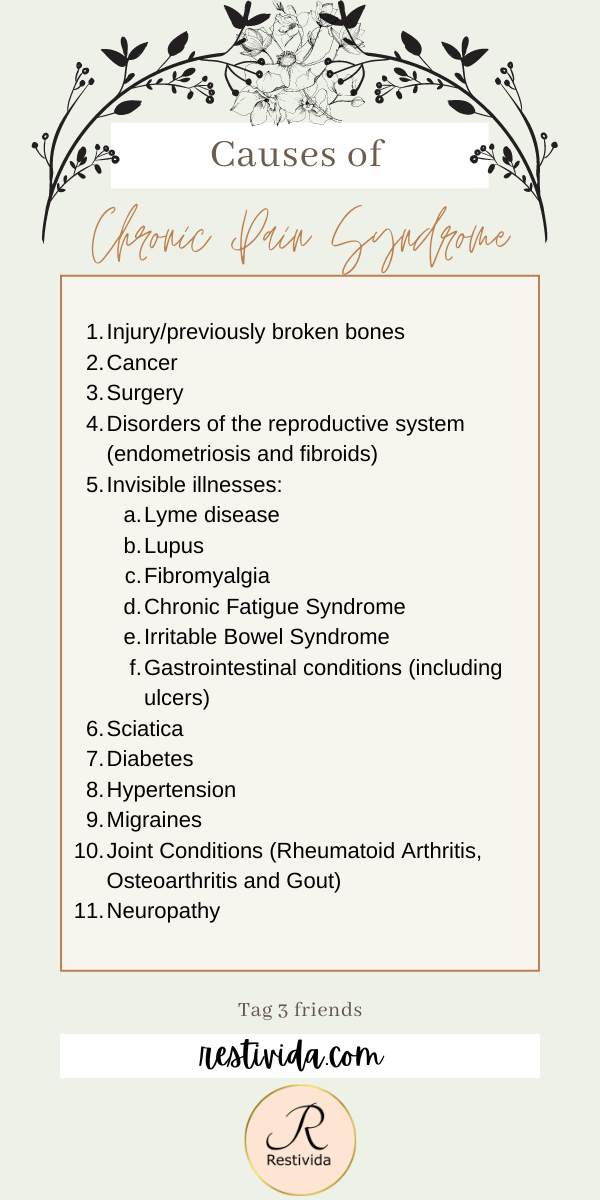
Causes of Chronic Pain Syndrome
- Injury/previously broken bones
- Cancer
- Surgery
- Disorders of the reproductive system (endometriosis and fibroids)
- Invisible illnesses:
- Lyme disease
- Lupus
- Fibromyalgia
- Chronic Fatigue Syndrome
- Irritable Bowel Syndrome
- Gastrointestinal conditions (including ulcers)
- Sciatica
- Diabetes
- Hypertension
- Migraines
- Joint Conditions (Rheumatoid Arthritis, Osteoarthritis and Gout)
- Neuropathy
The Science Behind Chronic Pain Syndrome
Although it is indeed true that your environment could affect the severity of the condition an important factor in Chronic Pain Syndrome lies in your genetics.
Studies have found that persons that have a difficult time recovering from injury or surgery are housing specific gene variants. Those that have migraine and cephalgia (headaches) have a single amino acid change in the protein that the body makes potassium channel regulators in the brain. If this protein is malformed, the regulation of potassium in the body becomes a bit difficult. Without potassium the body the muscles tend to contract longer and messages to the brain are delayed. Persons like this tend to be more susceptible to pain.
There are also genes that change the way the immune system reacts to pathogens which lends to chronic pain. In addition to these genetic variations causing one to be susceptible to pain there is also the element of chronification.
This is still being investigated but it could be as a result of genetics, medication, genetic changes early in life and brain plasticity. That means if your brain is adaptive enough it will be able to heal or reduce pain perception. So aside from the injury or illness there are two factors that can lead to Chronic Pain Syndrome.
- Your predisposition to pain
- If you are susceptible to the pain being “sticky” or not
Since gene sequencing is not a popular way to diagnose many illnesses as yet, your healthcare professional will need to rely on your symptoms and your pain dynamics, triggers, duration and intensity.
Before you get to your Doctor
Use the Free printable body form to write in all the symptoms that you’re experiencing. You can do this at home in a quiet space where you can think of all the symptoms that you’ve been feeling that may not be related but you’re still experiencing. It’s easier to have this ready to go and all the symptoms accounted for in one place than to finally sit in the office and forget some of the places that hurt; that really happens.
Aside from the pain, there’s also a symptom tracker that can help you to identify the pain dynamics. When it starts, what makes it worse, what makes it better… if it can even get better and how it changes and migrates throughout the day.
The pain tracker and the symptom tracker are great time savers especially if you have to go to a few different doctors and recount the symptoms over and over again.
If you’re more tech savvy check out this APP here. There’s a free and paid version as well as a “lite” version so you could decide what is best for you.
When you get to your Doctor
If you have all the symptoms tracked and all the information clear and ready to go your Healthcare professional will be able to make better decisions on follow up tests to be done and what part of the body to hone in on. These tests will give information on the function of the organs that they are associated with.
The metabolites, products and wastes will be observed and if the levels are not within “normal ranges” then more tests will need to be done. If you believe that your “normal ranges” are not typically normal for you then it’s ok to open a discussion with your healthcare provider about these results.
Accepting “normal range” but still experiencing significant and specific symptoms needs questioning especially if you’re on the lower or upper end of these “normal” ranges. Typically, scale is calculated based on the assumption that 95% of the population will fall within these ranges; but, you may be within the 5%.
You have the right to ask questions when it comes to your health and how these numbers are calculated, what exactly they mean and what they are looking for.
Images will look at your organs specifically. The specialist will check for foreign bodies, over growths and developmental and degenerative defects, size and position.
These imaging results will give an in-depth look at your organs and depending on where you are and your healthcare provider you will be able to get access to the newest technology.
They may suggest one or more of the following:
- Blood work
- Urinalysis
- Stool analysis
- Images
- CT scan
- MRI
- X-ray
- Ultrasound
Treatment for Chronic Pain Syndrome
Your treatment should be specific to you. At any point in your treatment you may ask for it to be modified if you’re not comfortable. Some medications require an “adjustment period”. You may see alternative treatment if you believe that is the way to approach your condition.
Understand that most Healthcare personnel will prefer to treat with medication because this is their specialty and this is what they know and believe will work. That does not make it true or false for your condition. You may choose to only take medication or you may use a multifaceted approach and incorporate other treatment methods. This is fine. Just keep you Dr. informed. You may choose an invasive or non-invasive methods or a combination of the two:
Invasive
- Acupuncture
- Scheduled injections (nerve blocker/epidurals)
- Surgery ***If it can be corrected by surgery then you’ll be taking the risk of correcting your condition by performing a procedure that may aggravate it more.
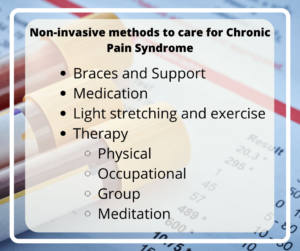
Non-Invasive
- Braces and Support
- Medication
- Light stretching and exercise
- Therapy
- Physical
- Occupational
- Group
- Meditation
Treatment for Chronic Pain Syndrome
Supplements
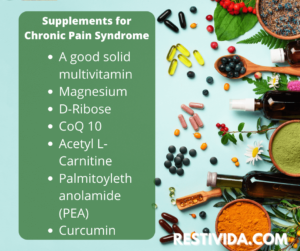
Supplements are great even for healthy persons. With the current condition of most urban areas in terms of pollutants and decreasing food quality due to poor soil quality from over farming, mono-cropping and use of growth enhancements it’s no wonder most of the food we’re eating aren’t as nutritious as it can be.
Some supplements support mood and nerve health while others are more specific to energy production as being in constant pain will suck your energy. Then there are those such as vitamin D that are specifically for pain reduction.
In addition, healing foods can enhance your progress and give some positive results and help you sleep. This is one of the major complaints of persons suffering from Chronic Pain Syndrome and one of the things that they want the most next to stopping the pain.
On your journey, it may not be possible to be pain-free which would be great but for most of us, but a functional and productive life and a new acceptable normal.
Supplements such as:
- A good solid multivitamin
- Magnesium
- D-Ribose
- CoQ 10
- Acetyl L-Carnitine
- Palmitoylethanolamide (PEA)
- Curcumin
Healing foods
- Bone Broth/Gelatin
- Ginger and Turmeric (Try our Golden Milk Recipe)
- Fenugreek
- Oily fish and nuts
- Olive oil
In conclusion, Chronic Pain Syndrome diagnosis is disappointing and somewhat devastating. The life you remember having where you were doing all that you could and then some is not over. There are three ways to go about living with any invisible illness.
The first is knowing as horrible as it may seem, you are alive and you can still spend time with your family. If you’ve lost your job you can look into other options to make money on your own time and energy.
The second is understanding what works for you and how your body works and reaction to medication, treatment and therapy treatments.
And Finally, the food that you eat is for your healing and energy production. It’s function is to support the body in performing its function. This is now more important for you than ever before.
Every morning you wake up is another chance to try again and keep trying. Live well!